

Medical Emergencies dial 999
Out of Hours: dial 111


Medical Emergencies dial 999
Out of Hours: dial 111

From time-to-time important alerts are issued by the practice or other local, regional or national organisations which are important to the health or security of patients.
Parents are being urged to be alert for the signs of group A streptococcal (GAS)
infections.
GAS is a common bacteria which can live harmlessly in our throats and on our skin. Sometimes it can cause mild illnesses like sore throats, occasionally more serious illnesses like scarlet fever and, albeit rarely, very serious diseases such as sepsis, pneumonia or bone infections.
Across Humber & North Yorkshire there has been an increase in cases this year, particularly in children under 10. Nationally, there have sadly been some deaths. Most sore throats and coughs are caused by viruses that will get better by themselves without needing antibiotics. However, we want parents to know what to look out for and when to seek medical care.
An NHS spokesperson explained: “Group A strep is usually something that is present and nothing to worry about, however what it can do is sometimes cause scarlet fever which is a common childhood infection that can be treated with antibiotics and need little medical assistance.
The symptoms of scarlet fever include a sore throat, headache, fever, nausea and vomiting and pinkish or red body rash with a sandpapery feel. On darker skin, the rash can be more difficult to detect visually but will have the same sandpapery feel to the touch. If your child has those symptoms, the best thing to do is seek medical attention by contacting your GP or NHS 111 as early treatment with antibiotics is important to reduce the risk of complications such as pneumonia or a bloodstream infection.”
While group A streptococcus bacteria usually only causes a mild infection producing sore throats or scarlet fever that can be easily treated with antibiotics. In very rare circumstances, these bacteria can get into the bloodstream and cause serious illness – called invasive Group A strep (iGAS). As well as an increase in notifications of scarlet fever, which is above the levels we usually see at this time of year, the Public Health Agency is also aware of a higher number of cases of iGAS being reported across the UK.
While iGAS is still uncommon, it is important that parents are on the lookout for symptoms of illnesses caused by group A streptococcus bacteria and seek medical advice so that their child can be treated appropriately and to help prevent the infection becoming serious.

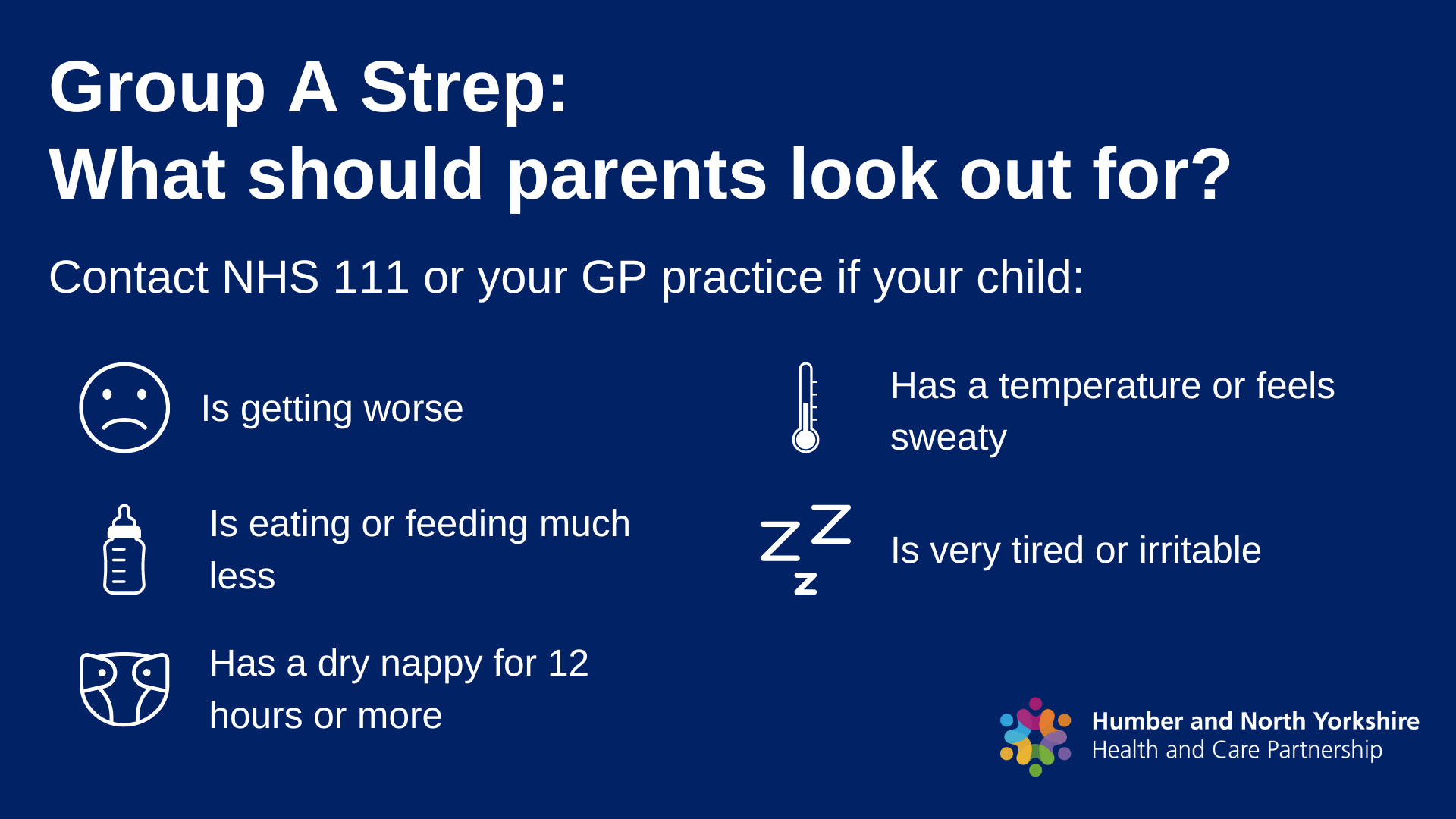
Parents are being urged to be alert for the signs of Strep A infections. This is also known Group A streptococcal (GAS) or invasive Group A streptococcal (iGAS) infections.
Especially in winter, there are a range of causes of sore
throats, colds and coughs caused by viruses that will get better by themselves without needing antibiotics or
medical intervention, meaning it not being necessary to contact your GP surgery.
Occasionally, Strep A can lead to more serious illnesses like scarlet fever and, albeit rarely, very serious disease such as sepsis, Pneumonia or bone infections.
Across Hull & East Yorkshire there has been an increase in cases this year, particularly in children under 10. Nationally, there have sadly been some deaths. We want parents to know what to look out for and when to seek medical care.
What to do if you suspect your child has scarlet fever:
Scarlet fever mainly affects children under 10, but people of any age can get it. In the early stages, symptoms include a sore throat, headache, and fever, along with a fine, pinkish or red body rash with a sandpapery feel. On darker skin, the rash can be more difficult to detect visually but will have a sandpapery feel.
We are asking parents to contact their GP if they suspect their child has scarlet fever, because early treatment with antibiotics is important to reduce the risk of complications such as pneumonia or a bloodstream infection.
Parents should contact their GP if they feel:
What to do if you suspect your child has scarlet
fever:
Strep infections are spread by close contact with an infected person and can be passed on through coughs and sneezes.
Please consider that emergency departments and GP surgeries are very busy. If you feel that your child can stay at home or be seen elsewhere, such as a pharmacy, please do so.
Know what to look for and when to seek medical care.
SIGNS & WHAT TO DO SCARLET FEVER
The UK Health Security Agency has confirmed that cases of monkeypox have increased recently but the risk to the UK population remains low.
Anyone can get mpox. Currently most cases have been in men who are gay, bisexual or have sex with men, so it's particularly important to be aware of the symptoms if you're in these groups.
Contact a sexual health clinic if you have a rash with blisters and either:
If you have an unexplained rash, please contact NHS111 or phone the practice to make an appointment.
Further public information is available - see below.
MPOX - WEBSITEMPOX ON NHS.UK